Contact Us Now ! 1-844-245-5633
Integrity Practice Solutions – A Professional Medical Billing Company.

At Integrity Practice Solutions, we are at the forefront of all the changes that are happening in the healthcare environment. We constantly learn and recommend ancillary services that a practice can add to their offerings to improve patients health and practice revenue.
Don’t get burned out! Let Integrity Practice Solutions handle your Internal Medicine coding and billing. Our specialists staff will submit your claims quickly, work on denials with complete follow up notes and get the revenue you deserve quickly in your bank account. We provide you 5 star billing service with a dedicated account manager and a team which will become an extension of your office. They will truly become your “Internal medicine billing department” and not just an outsourced vendor. You will have all modes of communications open with your team so your staff can get any information whenever they need it.
Our billers will review all the claims and send them out within 24 hours. Any missing information will be promptly discussed with the office so there are no delays in claims processing. We can use our software for billing or bill from your existing EHR. We have worked with Medisoft, eClinicalworks (eCW), Kareo, STI, OmniMD, Meditab IMS, OfficePracticum (OP), Healthfusion among many others.
Cash flow of your office is dependent on your claims going out in a timely manner. You cannot afford to have that stop when someone takes a vacation or has to take time off. With our size, your claims will never stop going out and your collections will always be worked on. You never have to worry about that.
We get paid only if you get paid. You get the benefit of having a specialized team of experts working on your account without worrying about training, vacation etc. If you go on a vacation, you do not have to pay any of your billing and collections staff.
You do not need to live in a vacuum!! We work with hundreds of providers and learn from the denials and push back that we receive from insurance. We learn from this and educate our practices so they do can get paid on the first time.
You and the staff you designate will always have full access to your data. We do not want to hide anything from you. When we do follow up, the notes will be attached to the patient chart and you can review them. We believe in 100% transparency.
It is your money and it is your right to work with whomever best serves your need. We do not impose any contracts. We are confident in our service that you will not find a harder working billing service provider.
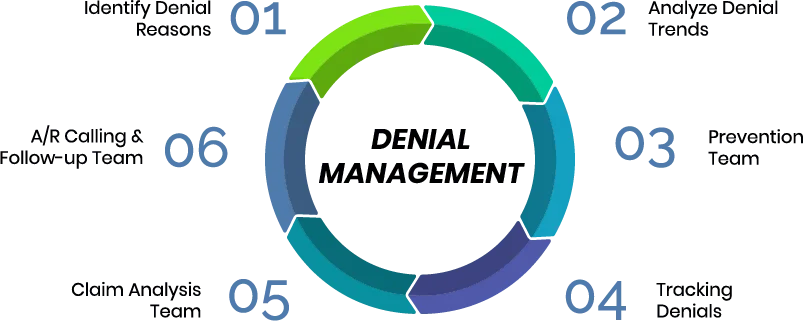
Denial management is the key to a successful revenue cycle program. Many companies claim to “automate” RCM but they fail to acknowledge that the problem in denials is the “intention” and not “technology”. There is no other alternative to being on the phone with the insurance company for hours on end and fighting for a claim to get paid. Nonetheless, smart billers learn from their interaction with insurances and pass on that knowledge to the offices they work with so they can take care of these “gottchas”. For e.g. many companies will deny a claim if you send a specific (e.g Lt knee pain) and unspecified pain diagnosis on the same claim.